Written by Dr. Ringpfeil
Lupus, short for Systemic Lupus Erythematosus (SLE), is an autoimmune disease that affects various parts of the body. In an autoimmune disease, the body’s immune system, which normally defends against infections, mistakenly attacks its own tissues. Lupus can impact any organ, but it most commonly affects the skin, kidneys, joints, and heart.
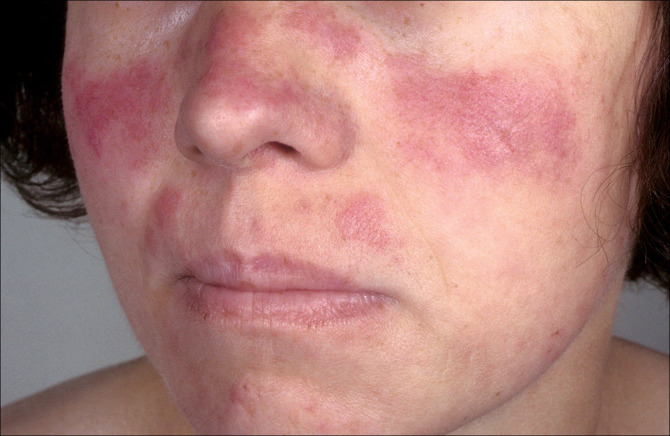
Approximately one in every 2,500 people may develop lupus, with females, particularly pregnant women, being more susceptible than males. The highest-risk population is individuals of African descent. A distinctive sign of lupus is a butterfly-shaped skin rash that may be accompanied by mouth and vaginal ulcers. Joint pain and extreme fatigue are also commonly reported symptoms, often resulting from anemia caused by a low count of blood cells. These symptoms occur due to increased inflammation resulting from the body’s immune system attacking itself.
Factors such as high levels of stress, hormonal changes, or exposure to sunlight can trigger flare-ups in individuals with lupus. Additionally, certain medications may cause adverse reactions in individuals with preexisting conditions, potentially promoting the development of lupus. Patients with other illnesses that cause a hyperactive immune system are more prone to autoimmune dysfunction. Genetic abnormalities in white blood cells may also contribute to the development of autoimmune diseases.
Diagnosing lupus can be challenging, but there appears to be a genetic component to the disease. Analyzing a patient’s family history may reveal past cases of lupus. Alongside a detailed patient history and physical examination, biochemical testing is necessary. Common tests include the “antinuclear antibody” and “antiphospholipid antibody” tests, which help identify the characteristic autoimmune features of lupus.
Unfortunately, there is currently no known cure for lupus, making it a lifelong (chronic) condition. However, there are ways to manage and treat the symptoms and flare-ups. Steroid treatment or immune-suppressing drugs are often prescribed to prevent widespread inflammation in lupus patients. Pain relievers are used to alleviate arthritis pain commonly associated with lupus, allowing most patients to continue their daily activities. Nonsteroidal anti-inflammatory drugs (NSAIDs) like Advil and Motrin can also help reduce fever during flare-ups.
Since stress can trigger flare-ups, it is recommended to involve friends and family in the treatment process. A strong support system can assist in managing doctor’s visits and coping with outbreaks. Avoiding intense sunlight and maintaining a healthy weight can also help reduce the frequency of lupus flare-ups.
Due to the complex nature of lupus, prevention methods are not currently known. Genetic factors play a significant role, and the best approach to minimize flare-ups is to prioritize personal health and regularly consult with a healthcare professional.
Given that lupus is a chronic disease affecting many individuals, the Lupus Foundation of America (www.lupus.org) has established local chapters across the United States. These organizations provide support for everyone living with lupus. Local doctors should have information on the nearest support group.
American Lupus Society
260 Maple Ct, Suite 123
Ventura, CA 93003
Tel: 800-331-1802 (Info Line)
805-339-0443
805-339-0467 (FAX)
Lupus Foundation of America, Inc.
4 Research Place, Suite 180
Rockville, MD 20850-3226
Tel: 301-670-9292
Tel: 800-558-0121
www.lupus.org
Patients ask Dr. Ringpfeil answers
Please feel free to use this form to ask our dermatologists questions about this treatment.